Why You Need a Physical Therapist on your Healthcare Team
Helen Sarandrea • July 24, 2020
With health in sharp focus as a result of the pandemic, now may be a good time to look at the
team of experts you have in place and see if there are any improvements you could make. You
probably have a family doctor, dentist, and optometrist. Maybe you have some specialist
physicians, a trainer, or a massage therapist. If a physical therapist isn't a part of your
healthcare team, you're missing out on taking care of a big part of your health. To understand
why you need a physical therapist, you need to understand what they do.
Physical Therapists Help You Do Things
The American Physical Therapy Association defines PTs as "health care professionals who
diagnose and treat individuals who have medical problems or other health-related conditions
that limit their abilities to move and perform functional activities in their daily lives." So physical
therapists help you do things that you have trouble with. That could be going for a hike, playing
with your kids, or getting through a day of work without pain.
Physical Therapists Reduce Pain
Chronic pain is a huge problem worldwide. A big part of that is low back pain. Statistically,
around 80% of people will have low back pain in their lifetimes. Physical therapists are trained to
treat pain without surgery or medications. If you have back pain, an arthritic knee, neck pain, or
an old injury that won't go away, a PT may be able to help.
Physical Therapists Keep You Healthy
The APTA goes on to say that "PTs work with individuals to prevent the loss of mobility before it
occurs by developing fitness- and wellness-oriented programs for healthier and more active
lifestyles." That means that a physical therapist can help you determine your risk for injury,
choose the right fitness program, and improve the quality of your life by improving your health
and ability to move.
Physical Therapists Can Help You Live Longer
It's well known that the risk of many of the leading causes of death can be reduced by exercise.
Some of these conditions would include heart disease, cancer, lung disease, diabetes, and
stroke. By helping you move better with less pain, finding the right exercise program, and
helping you to make healthy lifestyle choices, a PT could help you live longer.
Physical therapists have a unique set of skills and expertise that can do a lot to improve your
health and quality of life. If you don't have one, consider adding one to your healthcare team.
Physical therapists aren't just for people that are injured or have had surgery. Physical therapists can also help healthy people improve their fitness. Here are 5 reasons why you should consider seeing yours. You Want a Baseline When you see a physical therapist to improve your fitness, you'll get an assessment of your strength, range of motion, posture and movement patterns. This not only helps your physical therapist design a customized program just for you, it gives them a baseline to compare things to in the future should you start having pain or suffer an injury. You Want Expert Guidance Sure, other professionals could help with your fitness routine, but the fitness industry is not well regulated. Some certifications just require an online course and paying a fee. There are no licenses or other requirements to use many titles. Becoming a physical therapist requires at least a bachelor's degree and most PTs practicing today have a doctorate. Every PT has passed a national board exam and maintains a state license. That guarantees you that every physical therapist is a verified expert in human movement. You Want to Prevent Injury Physical therapists don't just work to heal injuries, they are also experts in preventing them. After a thorough assessment, a PT can help you design a program that will not only help you reach your fitness goals, but that can address any issues that increase your risk for injury. You Want Unbiased Advice Yoga instructors will want you to do yoga. Personal trainers will want you to come to their gym. Pilates instructors will want you to do Pilates. Strength coaches will want you to strength train. A physical therapist doesn't have a bias or vested interest as to what type of fitness regimen you choose. They are only interested in helping you reach your goals. You Have a History If you have some kind of history that affects your ability to exercise, a PT is the best person to help you design a fitness regimen. It doesn't matter if it's an old injury from athletics or work, back pain that comes up from time to time, COPD, arthritis or heart disease, a PT can help you safely work around it and meet your fitness goals.

While the coronavirus pandemic continues to be front and center in the news and in the thoughts of many people, other health issues have not gone away. People are still getting back and neck pain, overuse injuries and hurt while at work. Many of these people would benefit from seeing a physical therapist, but some of them are reluctant because of concerns over COVID19. That's understandable, PT clinics are busy places, with lots of people coming and going, right? They used to be, but things are different now. Just like every other business and public place, PT clinics have made changes to allow them to continue to serve patients while keeping both patients and staff safe. Here are some common changes clinics have made to reduce the risk of COVID spreading among patients and staff. Scheduling and patient flow ● Clinics have reduced the total number of people they see each day to allow for social distancing in the clinic ● Many clinics are using a staggered schedule to avoid people coming in at the same time ● Many clinics have implemented a "virtual waiting room" having people wait in their car and notifying them when their clinician is ready via a phone call or text message ● When possible, clinics may be using separate entry and exit points Treatment ● Clinics may be screening patients and staff as they enter the building using questions, temperature checks, or other means ● Clinics may have designated areas for each clinician and their patients to reduce contact between different groups of people ● Equipment will likely be spaced out further than you're used to and there may be less of it to allow for more distancing between patients ● Many clinics are leaning more heavily on telehealth when appropriate for patients to reduce the number of patients physically present in the clinic Physical therapists are medical professionals who were trained to deal with infectious diseases and keep people safe long before COVID-19 existed. By making changes throughout their workflows and patient experiences, physical therapy practices have reduced the risk of spreading COVID among their staff and patient populations, while continuing to deliver needed services to the public. If you are in need of PT treatment, but are hesitant to go into the clinic, give your PT a call and talk about what policies and procedures they have in place. To reduce or eliminate going into the clinic, ask about using telehealth either exclusively or in combination with in-person treatment. This is a time of uncertainty, but people are reacting with flexibility and creativity. Don't let concerns over COVID keep you in pain or from the treatment you need.

The weather is hot, the gym is closed, and you've been relaxing - enjoying the lazy, hazy days of summer. Taking a day off here and there is no problem, but if you've been consistently missing your regular run, bike ride, or gym session and notice some aches and pains showing up, you might have the beginnings of deconditioning. Deconditioning explained Exercise creates many changes in your body - your heart begins to pump blood more efficiently, your muscles use oxygen more efficiently, they contract in a more coordinated manner, and your body gets more efficient turning food into fuel to name just a few. Deconditioning is the reversing of these changes. Exercise is a "use it or lose it" kind of thing, and deconditioning is the process by which we "lose it." How long does it take to decondition? As with most things related to a system as complex as the human body, it depends. According to the ACSM, two weeks without exercise can lead to significant loss of cardiovascular fitness. Two to eight months of detraining can erase virtually all of your gains. As you detrain, cardiovascular fitness tends to decline first, with muscle strength declining later. Other factors are your age, and your exercise history. If you're younger, you'll probably lose fitness at a slower rate than someone older. If you've been consistently exercising for a long time, or at a high intensity, your losses will probably be slower than for someone who just started. Reversing the losses If you're just undergoing a period of increased time commitments at work or with family, using a shortened exercise routine can help minimize your losses. Even one session a week will help you keep most of what you've gained. Other options are to use shorter but more intense interval training sessions, or breaking up your activity into multiple short chunks during the day. If your layoff was longer, it may take just as long to retrain as it did to make the gains initially. If you're having those aches and pains due to inactivity or need help designing a safe program to either maintain your fitness or gain it back after a layoff, your physical therapist can help. Injury and illness are other common reasons for detraining. Your PT can not only help you recover faster, but they can also find activities to maintain your fitness while safely working around an injury or illness. ragraph

Because of the closures of physician's offices, stoppages of elective surgeries, and social distancing guidelines resulting from COVID-19, many people with pain or joint issues have had appointments or surgeries delayed. If you're one of them and you haven't seen your PT yet, you should. Here are some reasons why: Early PT leads to better outcomes Studies have shown that people who receive PT sooner have better outcomes, lower costs, are less likely to have surgery, use opioids or have unnecessary testing. Because back pain is so common, there is a lot of outcome data from people with back pain. A study of 150,000 insurance claims published in Health Services Research, found that those who saw a physical therapist at the first point of care had an 89 percent lower probability of receiving an opioid prescription, a 28 percent lower probability of having advanced imaging services, and a 15 percent lower probability of an emergency department visit. Unfortunately, only 2% of people with back pain start with PT, and only 7% get to PT within 90 days. Early PT saves money The rising cost of healthcare is well known and early PT is something that has been shown to reduce costs without reducing the effectiveness of treatment. A study published in the Journal of Orthopaedic and Sports Physical Therapy showed that patients who obtained physical therapy via direct access had significantly lower medical costs—an average of $1,543 less per patient than those who chose referral from a physician. They also had significantly fewer visits and spent significantly fewer days in care. Surgery may not be as effective as you think Many patients look to surgery as the fix for their pain, but surgeries aren't always as effective as patients believe. A large study looking at worker’s comp patients with back pain found that people who have surgery have a 1 in 4 chance of having a repeat surgery, a 1 in 3 chance of a major complication, and a 1 in 3 chance of never returning to work again. Recent large studies of arthroscopic surgeries for meniscal tears have shown no difference in outcomes between people who have surgery and those who don't. Other procedures with questionable effectiveness include kyphoplasty, vertebroplasty, and injections for nonspecific back pain. So, if you were planning on seeing your PCP or a specialist for an orthopedic condition or pain and you haven't seen a PT yet, you should consider making PT your first stop. You could end up getting better faster for less money and you might avoid riskier treatments like opioids or surgery.

How much thought have you put into the exercises you're going to use for your next workout? Did you choose them yourself, or did you find them on the internet or in a magazine? What's your workout designed for? Do those goals match yours? Are the exercises even safe for you? Using the wrong program can lead to wasting time in the gym, frustration, plateaus in progress and injury. Let's take a closer look at what goes into program design and the cost of getting it wrong. Exercise Selection There are many things to think about when choosing specific exercises. Machine vs. free weights, isolation vs. compound lifts, number of reps and sets, etc. Each one of these factors affects the results, so making the wrong choices could lead to wasting time working on the wrong things, limit your results or lead to injury. Technique If you choose the right exercises, but don't know how to do them properly you will again limit your results, or worse, end up injured. Poor technique leads to inefficient movement and limits the power your muscles can create. It also changes the load on your muscles, joints, and ligaments which can lead to pain and injury. Volume Volume is a way of thinking about how much work you're doing during a workout. Doing a few reps with a heavy weight or a lot of reps with a light weight could end up being the same volume. Same goes for running a shorter distance quickly uphill vs a longer run at a slower pace on flat terrain. If your volume is too great you won't recover well between workouts and create the possibility of injury. Too little volume and you won't see results. Progression If you've been doing the same exercises with the same weight and the same number of reps and sets, you're not progressing. Same goes if you jump on the treadmill for the same amount of time with the same settings each time. To make progress, things have to change and the program that works for your first 6 months won't work for you 2 years down the road. Designing an exercise program is a complex challenge with a lot of factors to consider. Most people have a history of injuries and don't have perfect movement in every joint which further complicates things. If you're not making progress or just want to make sure your workouts are as effective as they can be, have your physical therapist take a look at your program. Your PT can help design an individualized program to help you reach your goals while keeping you safe and injury free.

Medical diagnoses don't need much of an introduction. They're what you get from your doctor when you're sick. Examples would be influenza, diabetes, or hypertension. They describe the underlying problem that is causing your symptoms. When people feel sick, they know they need to go to the doctor and find out what's going on to get treated. We should treat movement the same way. If you're having pain when you move, can't do things you used to be able to - like get on and off the floor easily, or can't do things you want to do - like go for a bike ride or pick up a grandchild then you need to get a movement diagnosis. A movement diagnosis does the same thing as a medical diagnosis; it describes what's causing your difficulty with movement. Some examples would be difficulty standing from a chair secondary to decreased force production, scapular down rotation syndrome, or lower crossed syndrome. Diagnoses set the roadmap for treatment, so getting them right is crucial. Human movement is complex and is influenced by more than just your muscles and joints. According to the APTA, movement is impacted by the following systems: ● Endocrine ● Nervous ● Cardiovascular ● Pulmonary ● Integumentary ● Musculoskeletal Because of the complexity and interplay between these components of the movement system, getting a movement diagnosis correct is often very difficult. Physical therapists are experts in human movement with doctoral level training and should be your first stop for movement issues. Not only can a physical therapist provide an accurate movement diagnosis, they will also design a treatment plan to correct the underlying issues and help get you moving well again. References: http://www.neuropt.org/docs/default-source/default-document-library/movement-systemdiagnosis-in-neurologic-physical-therapy-where-are-we.pdf?sfvrsn=0 https://journals.lww.com/jnpt/FullText/2018/04000/White_Paper__Movement_System_Diagnose s_in.9.aspx http://www.apta.org/MovementSystem/ http://www.apta.org/MovementSystem/Template/
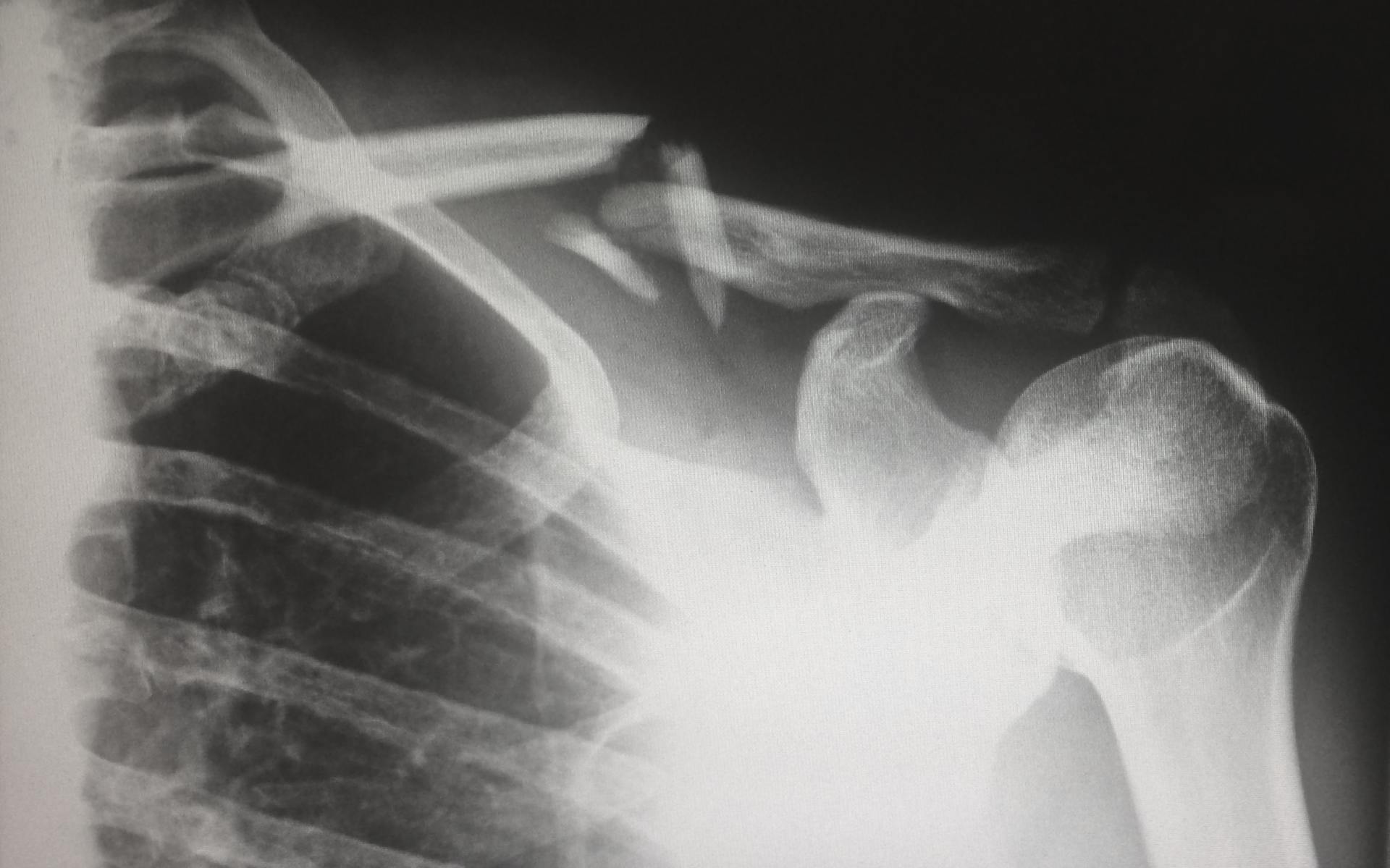
Physical therapists are experts in the musculoskeletal system, and typically use patient history and a good physical exam to come to a diagnosis and treatment plan. However, PTs are increasingly using diagnostic imaging as they become the practitioner of choice for musculoskeletal injuries. Many PTs have access to diagnostic ultrasound right in the clinic, and in some practice settings like the military, and certain ACOs, therapists have the ability to order imaging like x-rays, CT scans and MRIs. The research indicates that PTs are effective in using their ability to order imaging when it exists. A study of 108 imaging orders by PTs providing musculoskeletal primary care in a direct-access sports physical therapy clinic found that advanced diagnostic imaging was ordered appropriately in over 80% of cases. So, PTs are good at appropriately ordering imaging, but how does it improve treatment? A case study published in the July 2015 issues of the Journal of Manual & Manipulative Therapy gives a good illustration: The patient was a very active dentist who had chronic mid and upper back pain. He had a known history of benign neural tissue tumors of his head and upper back region, but no specific diagnosis for his back pain had been provided. After examination, the PT decided to start treatment for the patient's back pain, but also order x-rays and an MRI of the symptomatic part of the patient's spine. The MRI showed a previously undiscovered meningioma, or benign tumor of the membrane that covers the spinal cord. The benefit to this patient was that the PT could continue treatment without making referrals and waiting for someone else to order the images. Also, once the tumor was discovered, the PT could select exercises and manual techniques that would help the patient, but avoid putting stress on the area of the tumor. It also allowed the PT to educate the patient on fitness activities that would be safe and appropriate. The case study has a quote that sums up the benefits of imaging combined with PT nicely: "Orthopaedic physical therapists have high levels of musculoskeletal expertise and extensive knowledge of typical patterns and behaviors of musculoskeletal conditions. These competencies and experiential knowledge enable them to appropriately recognize situations requiring additional diagnostic screening for nonmusculoskeletal pathology. This case demonstrates how privileges to order musculoskeletal imaging studies assisted the physical therapist in providing optimal, patient-centered care. The physical therapist in this case was able to continue treatment without multiple referrals back to the medical provider to obtain imaging, and so provided more cost-efficient and convenient care." Reference article and case study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5046964/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4534847/

Think about the last time you made a big purchase, say $1,000 or more. Did you go out and buy the first thing you saw? Take one recommendation from somebody? Or did you research it, learn some things, compare it to other options, and select something that was right for you? Most people tend to be educated and research large purchases like cars, televisions, or the newest iphone. So why do we so often fail to do this with healthcare? By becoming more educated healthcare consumers we can go from passive patients who take the first recommendation that comes from a practitioner to an active consumer who weighs options and makes choices. Here are some questions to talk through with your practitioner the next time a healthcare decision comes up. What are the benefits or expected results? When a treatment or procedure is recommended, the patient often assumes that it will make them "better." But what the patient expects and what the healthcare provider expects are often two different things. For example, a patient having back surgery expects to be pain free after surgery. The surgeon probably doesn't expect that to happen. Outcomes from back surgeries are terrible. A large study of 1450 patients in the Ohio worker's comp system showed that after 2 years 26% of patients who had surgery returned to work. Compare that to 67% of patients who didn't have surgery. There was also a 41% increase in the use of painkillers in the surgical group. What are the risks and downsides? Patients want to hear about the benefits of a treatment, but they often don't ask or care about the risks. To be an educated consumer, you need to. If one treatment has a 3% edge over another, but has a high risk of making you itchy or causing frequent headaches, do you want it? Going back to the back surgery study from before, the researchers found a 1 in 4 chance of a repeat surgery and a 1 in 3 chance of a major complication. With surgery you risk infection, blood clots, complications with anesthesia, and a whole host of other things. These risks need compared with other treatments. In the case of back pain, physical therapy is a valid alternative with a much lower risk profile. You might have some soreness with physical therapy, you might sweat some and be challenged with exercise, but the risks of PT compared to surgery are minimal. What are the alternatives? Don't feel bad asking about alternative treatments. If you were looking at a certain car you wouldn't go out and just buy it. You'd at least consider the competitors and probably even test drive them. You should at least look at the other options in healthcare too. Maybe the first recommendation that your practitioner makes is the right one for you, but if you don't consider the alternatives you'll never really know. Why this treatment over the other ones? This is the question where the rubber meets the road. You've learned about all the options, now you can see if your practitioner is balancing the risks and benefits to make the right choice for you. Staying with the back pain example, research shows that more than 40% of people who seek care for back pain will not receive a treatment of known effectiveness. Back pain is also the #1 reason for opioid prescriptions, despite a 2016 recommendation from the CDC to avoid prescribing opioids for back pain, and opt for non-drug treatments like physical therapy. By asking for the rationale and carefully weighing options, you can avoid being one of the people who gets an ineffective treatment. What's it cost? This last question is becoming more important as patients bear an increasing share of the cost of healthcare. Even if you don't have a high deductible plan or hefty co-pays, by being financially responsible today, you'll probably see smaller price increases in your premiums down the road. That back surgery that we've been talking about? It'll likely cost between $60,000 and $80,000. So if we put the whole picture together, a patient who takes the first recommendation for surgery will have a $60,000 procedure that leads to a higher risk of disability, and a higher risk of long term painkiller use, while risking infection, and blood clots. Don't forget the 25% chance that you'll get to do it all again in a repeat surgery. Seems like a bad deal. An educated consumer would learn that physical therapy is a viable alternative to surgery with comparable outcomes, much less risk and lower cost. In fact, a large study of 122,723 subjects showed that people with back pain who got physical therapy in the first 14 days lowered their healthcare costs by 60%. It's easy to see why bargain shoppers love PT!

Recent research is showing that surgery might not be needed as often as we think. A large review estimates that 10% to 20% of surgeries might be unnecessary and that in some specialties such as cardiology and orthopedics, that number might be higher. The reasons for so many unneeded surgeries being performed are varied, but the most common are that more conservative options aren't tried first, or lack of knowledge by the operating physician. Physicians undergo long and rigorous training programs to become surgeons, but if they don't work hard to keep learning, their knowledge often stops growing when they leave residency. Recent research is showing that certain common surgeries aren't any better than a placebo. Two such examples are kyphoplasty - a procedure for spinal compression fractures, and partial meniscectomy - a procedure used to treat tears of the meniscus in the knee. If a surgeon hasn't continued to learn, they won't know that these surgeries often don't offer any more benefit than a non-surgical treatment and will continue to perform them. Every surgery, even "minor" ones carry risks. These include complications from anesthesia, blood clots after surgery, delayed healing of the incision, infection, and unintended damage to nerves or other organs near the surgical site. Some of these risks cause discomfort for a period after surgery and go away, but others can result in permanent disability or even death. For some patients and conditions, surgery is a great treatment option, but with all the associated risks, when surgery can be avoided, it should be. For musculoskeletal problems like back and joint pain, sprains, and strains, seeing your PT before a surgeon can help keep you out of the operating room and get you back to life without surgery. Studies have shown that physical therapy is just as good if not better than surgery for a multitude of conditions and carries less risk. Some examples would include rotator cuff tears, meniscal tears, spinal stenosis, low back pain, and osteoarthritis. Physical therapy can't fix every problem, and for some patients surgery is the best choice. However, research is showing that surgery isn't a cure-all, and is sometimes just a very expensive and risky placebo. In most cases, starting with physical therapy is the right choice, and for many patients, PT is the only treatment necessary.

Dealing with the pain and limited mobility associated with an injury or illness can be stressful for so many reasons. You might have questions like, “How long will I be sidelined?” and “What do I need to do to get better?” Or maybe you’re worried about how you’ll pick your children up from school, walk to the train for your commute or prepare meals for your family. These are all perfectly normal concerns. Luckily, there are some ways that you can gain control over the situation and ensure that you return to the activities you care most about—especially if physical therapy is part of your plan. What you can do before your very first appointment—and during physical therapy—to take control of that injury-related stress? First and foremost, it’s important to come prepared for physical therapy. And no, I’m not talking about dressing appropriately and arriving on time (or even better, 15 minutes ahead of your scheduled appointment). That stuff is important, of course, but there’s one thing you can do in the days leading up to your appointment that will set you up for success. Any guesses? I’m talking about starting a list. What kind of list? Well, every time that you feel pain in the affected area or notice an activity that is harder than it was pre-injury, add it to the list! And the more specific you are, the better. Here’s an example to help drive this point home: Let’s say that you’re recovering from a moderate meniscus tear and you have an appointment with your physical therapist in three days. Take notes on how your knee feels first thing in the morning after you’ve been off your feet. How does your knee react when you stand up from a chair—does it feel unstable? Or do you find that you need to clutch the back of the couch on your way to the bathroom? Sharing each of these details helps your physical therapist understand your limitations beyond the injury printed on your intake form. Now let’s take that list a step farther and add some details about the activities that you typically participate in on a regular basis. Let’s say that you normally play a weekly round of golf, spend your mornings weeding your garden or meet up with friends for a four-mile walk two evenings a week. These activities have become an important part of your life so let’s make sure that they’re factored into your list, perhaps in the “what you hope to get out of physical therapy” category. Painting a clear picture of how active you are—and what types of activities and sports you participate in—can help your physical therapist design an individualized treatment plan and to better help you on your road to recovery. Have you been to physical therapy lately for an injury? Did you find anything else that helped maximize your time in rehab or that improved communication with your physical therapist?

Share On: